Abstract
Background: Individuals with sickle cell disease (SCD) are at risk of severe COVID-19 infection. Those with SCD are also known to be at risk of venous thromboembolism (VTE), with numerous mechanistic pathways likely at interplay. In general, prior studies indicate that COVID-19 infection is associated with a thromboembolic risk. However, it is unknown if COVID-19 infection increases the already high risk of VTE for individuals with SCD. Given the preexisting risk for thrombophilia associated with SCD, we hypothesized that COVID-19 infection would further increase the risk of a venous thromboembolic event. In this study, we leverage electronic health record data to determine, at a population level, whether individuals with SCD hospitalized for COVID-19 have higher VTE rates when compared to hospitalization for any other cause.
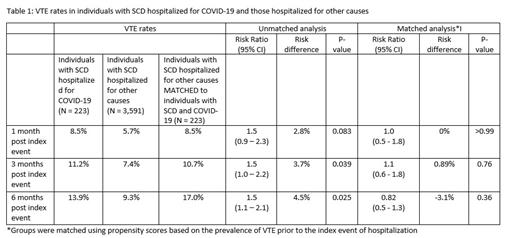
Method: Using electronic health record data from a multisite research network, TriNetX (years 2010 - 2020) we identified two mutually exclusive cohorts of individuals with SCD between Jan 20, 2020 - Dec 31, 2020: 1) those with hospitalizations related to a diagnosis of COVID-19 and 2) those with hospitalization for other causes. COVID-19 related hospitalizations were defined as admissions occurring within a month of COVID-19 diagnosis. Overall, individuals were considered to have SCD if they had 3 or more instances of ICD coding for SCD during the time frame of years 2010 - May 20, 2021 and did not have any ICD code for sickle cell trait. The outcome of interest was VTE, which included either deep venous thrombosis (DVT), pulmonary embolism (PE) or both. We determined the VTE rates at 1 month, 3 months and 6 months post hospitalization. The VTE rates between the two groups were compared using measures of risk difference and risk ratios, along with the respective 95% confidence intervals. We also matched the groups using propensity scores based on the prevalence of VTE prior to the index event of hospitalization and compared the respective outcomes.
Results: Within the TriNetX network, there were 223 (59% females) individuals with SCD hospitalized due to COVID-19, and 3,591 (54% females) hospitalized for causes other than COVID-19. Individuals with SCD hospitalized for COVID-19 were older than individuals with SCD hospitalized for other causes (mean age: 29.4 yrs, sd = 16.4 vs 26.3 yrs, sd = 16.8, p value = 0.006). A significantly higher proportion of individuals hospitalized for COVID-19 had a prior history of portal vein thrombosis (4% vs ~0%, p-value <0.001), phlebitis/thrombophlebitis (4% vs 2%, p-value = 0.026) and other VTE (16% vs 10%, p-value = 0.008). There were no significant differences in sex or proportion of those with prior history of PE between the two groups. Table 1 shows the VTE rates observed in the two groups 1, 3 and 6 months post-hospitalization, respectively. VTE rates were higher among individuals with SCD hospitalized for COVID-19 than among individuals with SCD hospitalized for other causes. After matching for previous history of VTE, individuals with SCD hospitalized for COVID-19 infection did not have significantly higher VTE rates compared to individuals with SCD hospitalized for other causes at any of the time points evaluated.
Conclusions: These data suggest that immunothrombosis accompanying SARS-COV-2 infection in individuals with SCD does not exacerbate the underlying known thrombophilia associated with SCD and provide support for current clinical guidelines in this population. Future prospective studies controlled for anticoagulant therapy exposures may provide more direct evidence to guide thromboprophylaxis in this unique population.
No relevant conflicts of interest to declare.